Faculty Spotlight: Larry Leeman
By Leslie Linthicum
He has also developed an interest in how psychedelic compounds can be used as medicines.
Putting those two interests together, Leeman is embarking this Spring on a study of how talk therapy combined with the use of MDMA (the compound in the party drug known as Ecstasy or Molly) might help new mothers recover from PTSD and opioid use disorder.
Mirage sat down with Leeman to talk about his research and the broader spectrum of clinical trials involving psychedelics that are being undertaken at UNM and across the country.
Mirage: I’d like to talk about the ‘psychedelic renaissance.’ There was a real explosion of research into the therapeutic potential of LSD and other psychedelics in the 1950s and 60s and then the research really was shut down for over 20 years. Rick Strassman in Psychiatry rebooted psychedelic research with his work with the psychedelic DMT at UNM in the 1990s. Now there’s Michael Pollan’s bestseller, “How to Change Your Mind.” And people are microdosing and there seems to be a new push for medical research using psychedelic compounds.
Leeman: When people describe a psychedelic renaissance, they tend to be talking about that from a Western and Anglo perspective. And I think it’s important, especially in New Mexico, to acknowledge that the use of psychedelic therapies dates back millennia in the Indigenous populations throughout the hemisphere. This wasn’t invented in the 70s.
Mirage: Noted. Research is about asking questions. What questions about the use of psychedelics interest you?
Leeman: I’m first and foremost a physician clinician. I’m very active in maternal and child health, delivering babies, taking care of people with addiction. And so a burning question for me is can these compounds help with addiction? Can they help with trauma? Can they help with PTSD? Preliminary research suggests yes, at least for MDMA for PTSD. But then, it gets deeper. It gets into what is it that’s effective about these? Do these psychedelic-assisted therapies work? If they do work, what are the psychological mechanisms? What is the best type of accompanying therapy? What are the biological mechanisms? Are there ways to develop new compounds?
Mirage: In these studies, using MDMA, psylocibin and ketamine along with psychotherapy, is it less about the emotional or psychological experience of having the drug on board and more about what that does in terms of the therapy that occurs?
Leeman: So the simple answer would be, we don’t know. We don’t know how important what you went through during the experience is. Most of us think it’s important, and that it forms the background for what we call the ‘integration,’ where insights that have been learned and processed can be integrated into one’s behaviors and one’s daily life. But that needs to be studied more.
Mirage: People who use psilocybin and MDMA recreationally report an increased sense of connection — connection to other people, to themselves, nature, the universe. How important is that aspect in your therapy?
Leeman: You’re talking to someone who’s an addiction medicine doctor.
There’s a quote that’s been used in the past that addiction is the opposite of connection. People that are addicted have a very narrow aperture. Eventually, it basically comes down to you and your substance, and that may be the only thing that you’re focused on. Almost everything else may be being manipulated to get your substance, and you will lose connection. I view connectedness as having multiple levels. One is the inner sense of connectedness, that we’re in touch with our own emotional feeling, self- awareness, our somatic state. The next level would be connectedness with your family, your partner, your community, your friends. And then the other level gets broader — our connection with the world or the universe. Those are three levels, some of the scales, that we’re using to look at that. A lot of this is theoretical.
We need to see what actually is associated with improvement in mental health and behavioral change. Because if we can figure that out, there’s ways to achieve some of these states without drugs. There are ways to achieve some of these states through meditation, there’s even forms of breathwork that you can use to facilitate these states of consciousness.
Mirage: So let’s talk about the study that you’re undertaking. MDMA-assisted therapy for helping relieve PTSD in postpartum women who are opioid dependent. What were your experiences at Milagro that led you to this research?
Leeman: When I first started working in addiction and pregnancy, I was taking care of the babies that had neonatal opioid withdrawal syndrome. And then that expanded to interest in the prenatal care and the childbirth. Part of what I saw is that a large proportion of the people we worked with who we were able to get stabilized, usually with the help of medicines including buprenorphine or methadone, and through the pregnancy and initial postpartum time. But then I started seeing people coming back. Two years later they were pregnant again and back on opioids despite having achieved stopping use during and immediately after the last pregnancy, which is what they wanted. Sometimes we can all be slow to understand, but eventually I got it. Okay. We’re helping with the addiction. We’re helping with the craving for the opioids. But we’re not getting to what causes the addiction. I wasn’t doing anything to help them with their trauma, which is causing this self-medication with opioids. We weren’t actually treating the trauma. And PTSD has been notoriously difficult to treat, especially in the people who had it for a long time. So I started doing some exploration of what are the ways of treating that? One of the innovative ways was with MDMA-assisted therapy, which has demonstrated high levels of success, where about 70% of people after the course of treatment no longer meet the criteria for PTSD, about twice the proportion of people that are using a placebo in studies. The University of New Mexico supported me in doing a sabbatical in psychedelic- assisted therapies and addiction at Madison, Wisc. I was able to become a researcher and a therapist on their Phase 3 MDMA study to learn how to use MDMA-assisted therapy. One of the goals of that sabbatical was to come back here and bring this research and therapies to New Mexico.
Mirage: Why are you choosing to study a population that has PTSD and substance use disorder and recently had a baby?
Leeman: Yeah, so what’s the reason for studying these complicated people? Well, I guess there’s two ways of answering. First, that’s the people I’m taking care of. But on a deeper level, this is our future. In the families I work with I had trouble identifying anyone in the family that didn’t have addiction. It goes back multiple generations.
Mirage: Is the goal of this to have women who are having babies have safer and healthier experiences because they’re no longer using opioids? Or is it to have them have better experiences with their children because they’re having less trauma, less PTSD, and therefore more connection?
Leeman: All of the above. But we think that may happen in sequence. So what are our actual research objectives? One of them is seeing, can you treat PTSD in people that have opioid use disorder successfully with MDMA? The next part, which is major, is decreasing resumption of opioid use. We know that within the first 12 months after childbirth, over 50% of people resume use. In our study we will be watching people out to six months after treatment to see if they’ll be less likely to resume use of opioids. Resuming use of opioids has all sorts of bad outcomes. As you mentioned, it can affect your parenting. It can actually affect custody of your children if it gets bad enough. We see many pregnant postpartum people lose custody of their children. That’s a major life trauma. Another concern, unfortunately, is that a common time for overdose is postpartum. The last goal of the study is the most exploratory, which is looking at how the MDMA – assisted therapy affects parenting. We have a series of assessment tools that we’re using — the maternal-infant bonding assessment and a video assessment where we observe the study participant and we watch how they’re interacting with their baby. It’s based on the idea that trauma affects bonding and attachment.
Mirage: What’s the tie between trauma and addiction?
Leeman: When you look at causes of addiction, the roots are often in adverse childhood experiences. When we think of adverse childhood experiences, they can be various forms of trauma – Big-T or Little-T trauma. Big-T trauma is something major that happened- your parent is shot, you’re in a war, you experienced sexual abuse — those are all Big-T trauma. But the addiction is also associated with other kinds of trauma. You have a parent who’s emotionally absent and don’t experience feeling of love and safe attachment. Those are deep rooted. Our hope is that early in the lifespan of the mother and baby that we may be able to affect that. This is very preliminary, but we’re going to look at that both from the questionnaires and from the videos and from qualitative analysis by interviewing the mothers six months after completing the MDMA-assisted therapy. And if we do show that there’s a benefit, then we have a new treatment to help with intergenerational trauma. As we see commonly in New Mexico we are kind of in a cycle here. I call it a cycle of despair. People experience trauma, they have addiction, the addiction gets them exposed to more trauma, and the cycle continues.
Mirage: This is about the mother connecting with her trauma in a safe way and also encouraging connections between the mother and her baby. And MDMA is a possible avenue to both?
Leeman: You and I were talking earlier about connectedness, bonding that would be associated with being a new mother. MDMA is a complex chemical, and it works in different ways, but it does increase oxytocin release, which is the same chemical that is involved in maternal- infant bonding. The way MDMA- assisted therapy works, to the best of our knowledge, is that when the therapy is done in a safe container it allows people to process their trauma without the feeling of reexperiencing the trauma.
Mirage: While you’re doing this, are you actively doing therapy? Like asking them questions? Or are you letting this subject just experience the feeling?
Leeman: Great question. During the preparation system sessions, we’re getting to know them, we’re talking about their life. It’s relatively loosely structured and patient-led during the session itself. When you take people who’ve had significant trauma and you give them a compound that temporarily allows them to look at their life and that trauma without getting triggered by those feelings, I do not have to go, ‘Tell me about your trauma.’ People do it themselves. What happens during the session, which usually lasts about five hours, is they have a time when they’re lying down, they have eyeshades on and they have headphones with music. And then they speak with the therapists and share their experience. Commonly they go in and out — times of wearing eyeshades and times of talking. There’s an inner processing, where they’re usually thinking about these sorts of things. and when people come out of it, they talk and share about their experience. And what they’re doing through this is reprocessing the trauma, they’re kind of reframing it. It’s hard to heal from something, if every time you think about something, you go into fight or flight or freeze responses, then you really can’t process that. And we are giving people a temporary holiday from those trauma pathways. But we’re giving them that holiday in a way that they come out and talk about the trauma and have the potential to heal through that.
Mirage: Is there still a stigma to this type of research, especially in the National Institutes of Health, which is a major funder?
Leeman: I think the stigma didn’t originate in the NIH. I think the stigma originated in society.
There’s still a lot of collective cultural memory from the time of the 1970s, when these became part of the culture wars. And in the late 60s and 70s there was an overenthusiasm of some thinking that using these substances was going to change the world. I think we’re societally reframing that to ask, what is a substance of abuse and what is potentially a therapeutic medicine? There are very promising studies that are out there — psilocybin for major depression, MDMA for PTSD, psilocybin for alcohol or tobacco use. As those have come out, the NIH has become interested in and welcoming of research into psychedelic-assisted therapies. They’ve looked at the studies, they’ve had conferences, and they’re starting to support that. It’s still small, but hopefully, there’ll be a lot more. I’m optimistic that, at UNM, we’re in a position to be at the forefront of that area, particularly with addiction and trauma, because we are a major epicenter of opioid use disorder. And most of the early studies of psychedelic medicine occurred with white males. So, we want to also make sure this is being studied in a multicultural population.
Spring 2024 Mirage Magazine Features
Understanding Headwaters
Understanding HeadwatersJan 7, 2025 | Campus Connections, Spring 2024 A $2.5 million grant from...
Read MoreNo Je or No Sé?
No Je or No Sé?Jan 7, 2025 | Campus Connections, Spring 2024 In his research, Associate Professor...
Read More‘A New Pair of Eyeglasses’
‘A New Pair of Eyeglasses’Jan 7, 2025 | Campus Connections, Spring 2024 Nancy López,...
Read MoreSenate Judiciary and Mental Health
Senate Judiciary and Mental HealthJan 7, 2025 | Campus Connections, Spring 2024 Colin Sleeper, a...
Read MorePlant Power
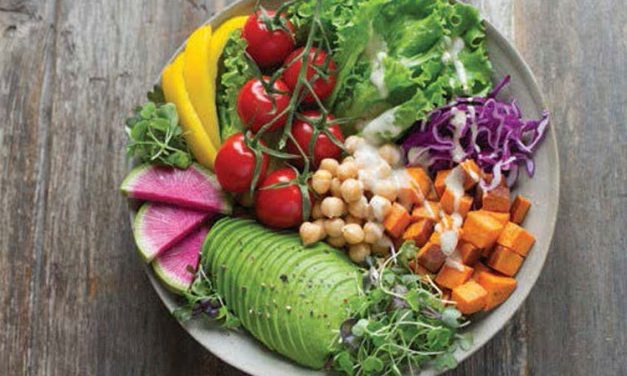
Plant PowerJan 7, 2025 | Campus Connections, Spring 2024 More people are choosing plant-based...
Read More